RCM Performance Suite
Elevate revenue cycle results with precision intelligence and full audit traceability.
Challenges
Invoice operations break at scale. Agentic AI is required to restore control, accuracy, and speed across the invoice lifecycle.
Fragmented Invoice Data
Invoices arrive across emails, portals, ERPs, and scanned documents. Data stays siloed, inconsistent, and difficult to standardize in real time.
Slow Approval Cycles
Approvals move across disconnected systems and stakeholders. Delays result in missed SLAs, late payments, and strained vendor relationships.
Manual Validation Overload
Line-item checks, tax validation, and PO matching depend on manual effort. Exceptions accumulate faster than teams can review and resolve.
Limited Audit Traceability
Invoice decisions lack end-to-end visibility and context. Audits require manual reconstruction instead of instant, explainable records.
What Defines Us
Intelligence tailored for revenue integrity and operational clarity.
RCM Performance Suite is engineered for healthcare finance, billing ops, and revenue integrity teams. It consolidates patient encounters, claim forms, and medical records—regardless of format—and surfaces structured, decision-ready insights.
Anomalies and denial risks are flagged and ranked, with full traceability back to their origin in claims or clinical documentation. A rule engine applies your payer or policy logic, while performance dashboards visualize key metrics—turnaround times, denial trends, revenue leakage. As your team reviews and corrects, the system learns and refines future predictions.
The result: fewer denials, faster reimbursement cycles, and data you can audit, trust, and act on.
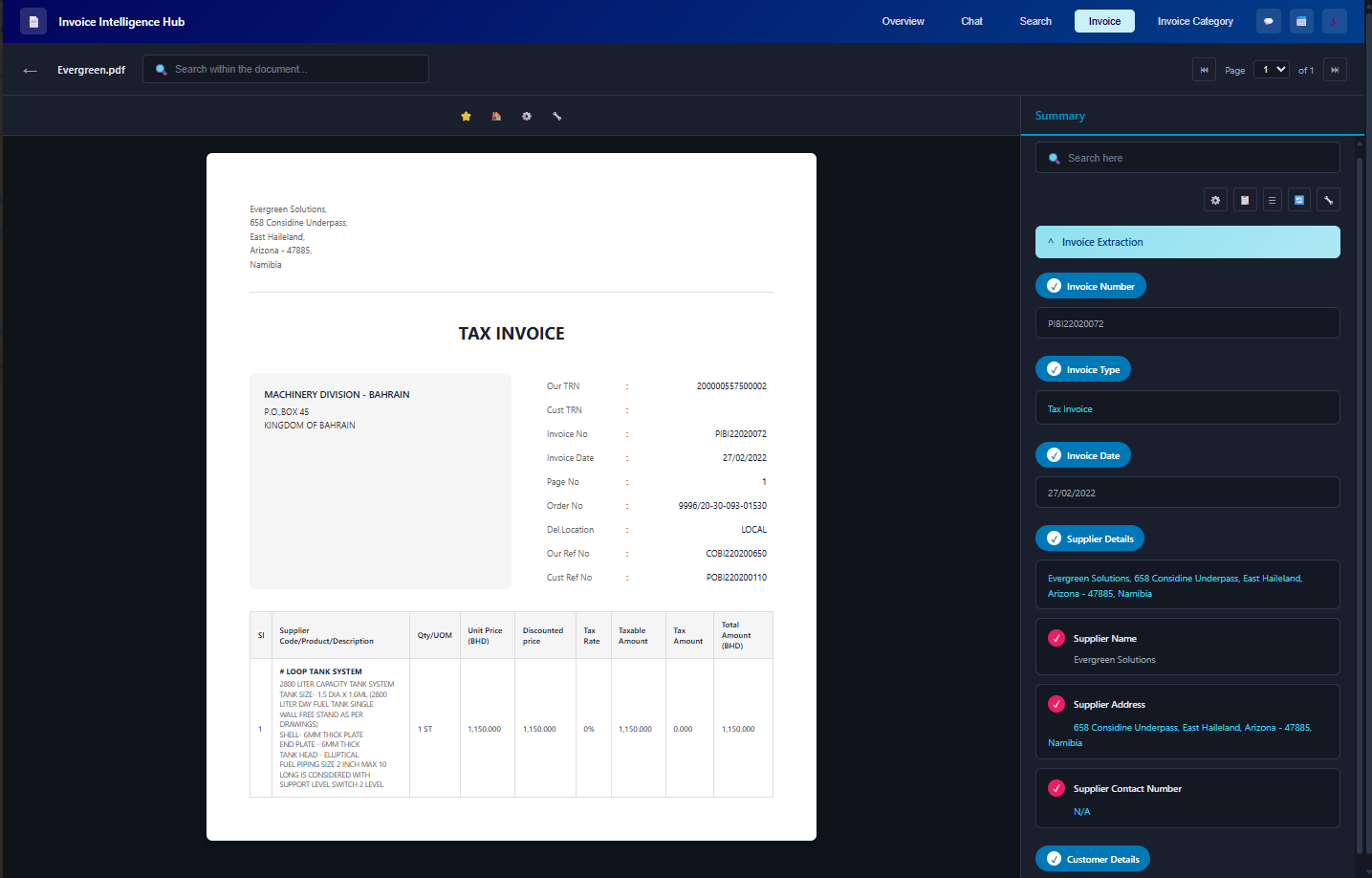
Template-free, Accurate Invoice Data
Extraction — in a Few Clicks
Extract claim and patient data across formats, detect anomalies, prioritize interventions, and monitor RCM metrics—while maintaining trace links to original documents and ensuring governance.
Accuracy
Process Efficiency
Reduced Time
Claims Files Throughput
See RCM Performance in Action
Watch how the suite transforms claims and health records into structured insights—driving measurable uplift in cycle efficiency and revenue integrity.
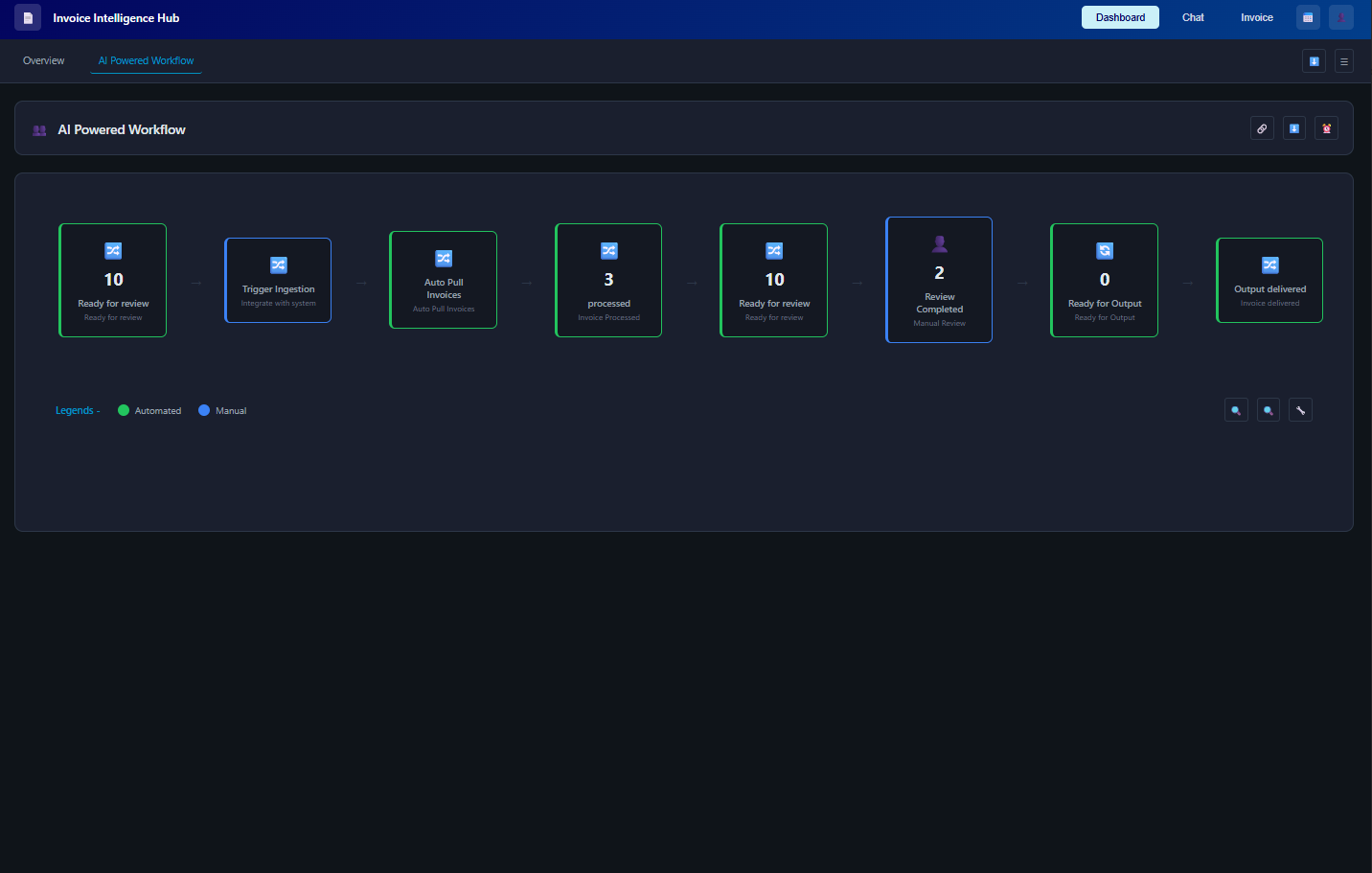
AI Workflow Automation
Automate the entire invoice processing workflow from capture to payment. End-to-end automation
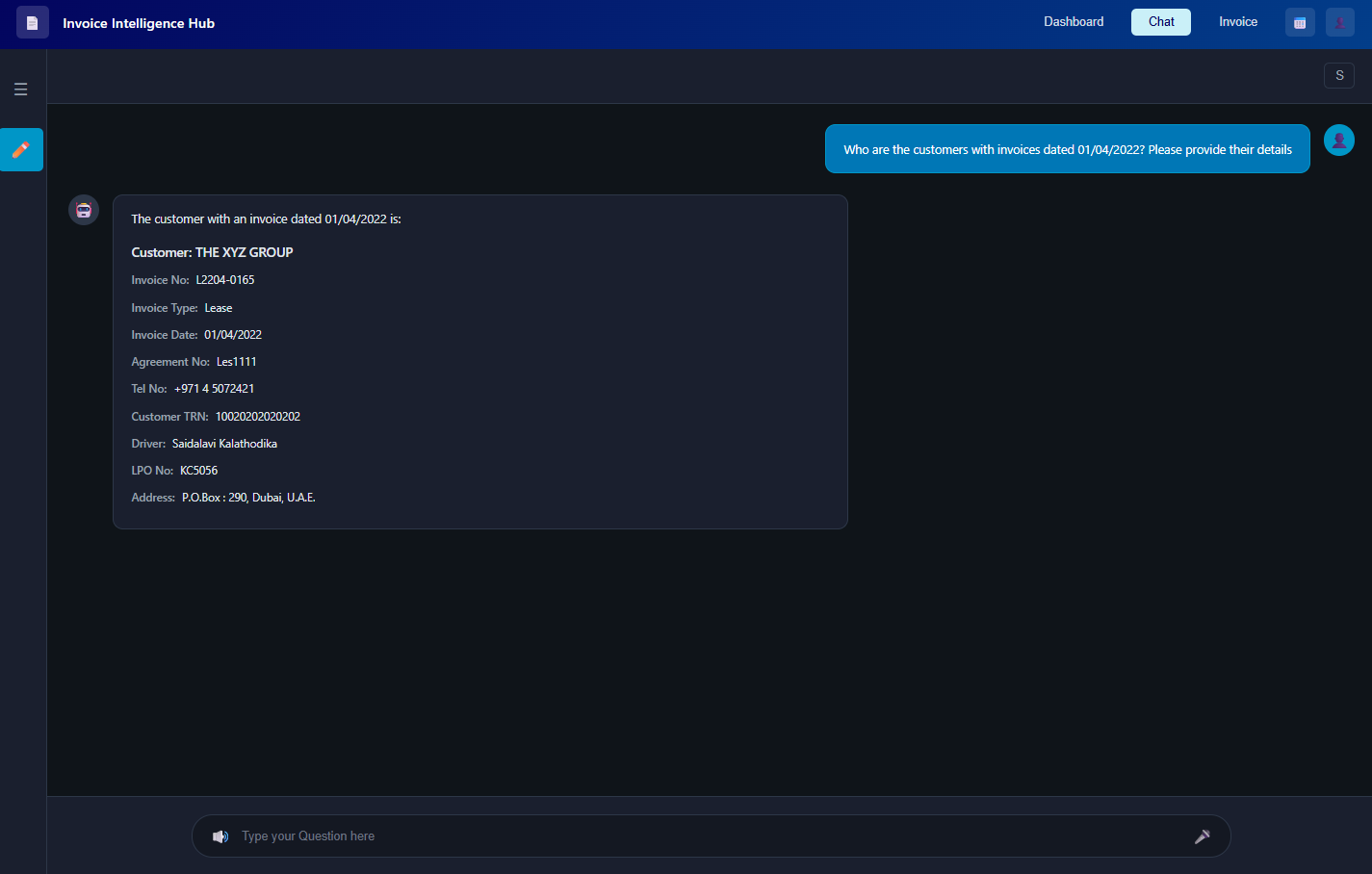
Intelligent Chat Interface
Interact with invoices using natural language queries. Ask questions, get insights
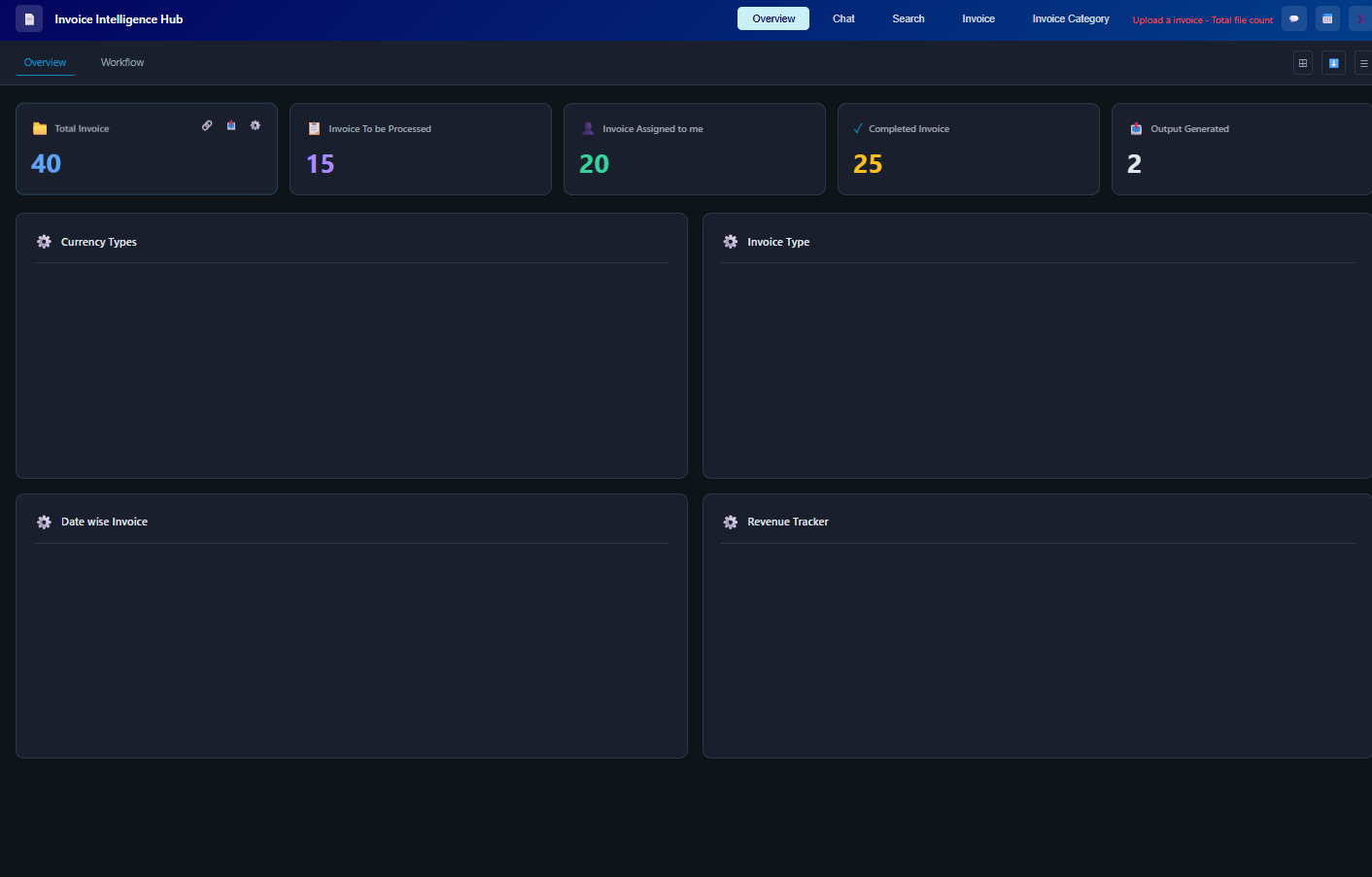
Real-time Dashboard
Monitor invoice processing metrics and status in real-time. Live updates and analytics
Detailed Invoice Summary
Get comprehensive summaries and validation of invoice data. Accurate extraction and validation
Get the answers you need
Find clarity on our solutions, capabilities, and how we can support your business.
RCM is a critical, time-consuming and administratively heavy process that includes patient registration, insurance billing, verification with payors, coding the claim, payment and collection.
Errors and delays due to manual entry or checks across high volumes of documents leads to poor patient satisfaction; and delays in collections for the healthcare providers.
With a huge number of payors (over 900 in the US), health plans, validation checks required and regulations to comply with – health care providers outsource this critical back-office process to RCM service providers – who deploy large teams to handle this.
Pre-processing a claim filed needs to be done in a stipulated time frame – and this poses a challenge when done manually.
Automation of the RCM process enables RCM service providers turbocharge the entire process – handling claims in minutes with ~100 accuracy – they are thus able to increase the volume of records handled with the same time (nearly 3X)
Health care providers can also leverage automation to reduce manual efforts and streamline their RCM process.
The Botminds AI platform can handle all key financial statements in multiple formats, reporting/accounting standards and filing types across geographies - Balance sheets, Income statements, cash flows, Annual reports, SEC filings (10Q, 10K, 8K etc.); tax forms; Personal financial statements etc.
Botminds can handle any PDF documents (scanned or digital) - handwritten and/or printed. In addition, the Botminds AI platform can extract relevant payor, provider or other related unstructured data from web pages, if any.
In case of SaaS model, the data is highly secure with 2FA and role-based access controls in place. Botminds platform was built with high degree of data security in mind.The Botminds AI platform can also be deployed in a private cloud environment for our clients – this ensures that documents and data never leave the client’s environment.